This project is now in update mode. Check back regularly to see how things are progressing.
ThinkSepsis: Development of a prehospital alert tool
Although their campaign has concluded, if you would still like to make a donation to ThinkSepsis, you can always do so here.
------------------------------------------------------------------------------------------
Sepsis is a life threatening condition that arises when the body's response to an infection injures its own tissues and organs. Sepsis can lead to shock, multiple organ failure, and death especially if not recognized early and treated promptly. Sepsis remains the primary cause of death from infection despite advances in modern medicine, including vaccines, antibiotics and acute care.
Our Problem:
More than 2 million Americans are hospitalized each year with sepsis – and many have never even heard of sepsis. Sepsis is a leading cause of death in the intensive care unit (ICU) and the hospital, where one in five sepsis patients do not survive. Almost 20%! Most sepsis patients are brought by ambulances to the hospital, and not enough emergency medical services (EMS) providers are knowledgeable about the condition. Patients don’t complain of being “septic." As a result, many delays occur in the treatment of sepsis, and a critical window for treatment may be missed.

The Solution:
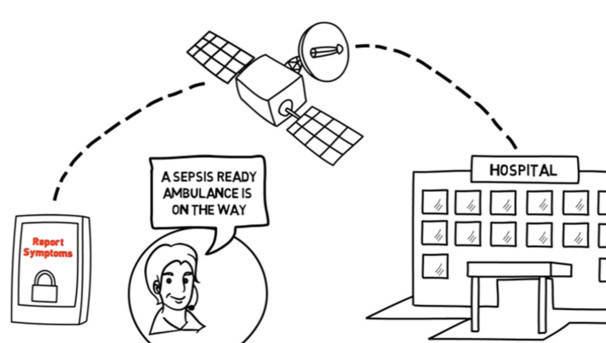
To equip frontline EMS providers with an objective app for sepsis recognition, preventing unnecessary delays in treatment. The handheld, wireless tool being developed by the ThinkSepsis team will empower first responders to report sepsis symptoms early and facilitate the transfer of vital data to medical command physicians who can activate a system of sepsis care.

Why This Matters:
The risk of death rises by seven percent each hour sepsis goes untreated. Currently, fewer than 30% of EMS cases with infection are identified in local EMS systems. The ThinkSepsis tool could greatly increase the recognition of sepsis and speed up treatment.
Current Progress:
Over the past year, our interdisciplinary team made up of local EMS, experts in sepsis, patients, and software developers at Truefit™ has worked together to create an initial prototype. The tool is based on a user-centered design process that focuses on the patient experience, minimizing user error, and allows secure data transfer in real-time. The application will be ready for pilot testing in mid-2015.
Our progress is made possible thanks to partial funding from the Pitt Innovation Challenge (PInCh) in May 2014, a competition designed to generate innovative solutions to challenging health problems.
How Your Support Will Help:
Your donation will be used to equip participating Pittsburgh-area EMS trucks with the necessary devices and wireless contracts to move forward with the pilot test. Our goal of $4,000 is based on the cost to fully equip 6 of the 12 trucks that will participate in the test. Your donation will help directly support the research infrastructure and hardware necessary to make this pilot test successful.
-
Cost to equip one truck with the full sepsis alert system: $665
-
Secure wireless device (16GB iPad Wi‑Fi + Cellular): $530
-
Wireless contract: $35 per month for 3 months ($105 per truck)
-
Protective case and cover: $30
-
Throughout the campaign, we will provide regular updates on our progress so that you can see how your support is making a difference.
Long-Term Vision:
Our hope is that this sepsis care system will not only be feasible and widely applicable to EMS agencies that serve the Pittsburgh area, but will also serve as a model for regions outside of Southwestern Pennsylvania.
Please Share Our Message:
If you have a friend, family member, colleague, or know anyone you think would be interested in or benefit from learning more about ThinkSepsis, please share this project with them. The University of Pittsburgh and the ThinkSepsis team are grateful for the generous support of donors, and we are passionate about educating the community about the dangers of sepsis.
Thank you for your support!
OUR TEAM
Christopher Seymour, MD, MSc
Assistant Professor, Departments of Critical Care and Emergency Medicine
See bio in "project owners" section at top of page
Derek C. Angus, MD, MPH, FRCP
Distinguished Professor and Mitchell P. Fink Endowed Chair, Department of Critical Care Medicine, University of Pittsburgh and UPMC Health System

Dr. Angus is Distinguished Professor and Chair of the Department of Critical Care Medicine at the University of Pittsburgh School of Medicine and UPMC Health System. He holds secondary appointments in Medicine, Health Policy and Management, and Clinical and Translational Science. He completed his medical school and residency training at the University of Glasgow and fellowship training at the University of Pittsburgh. Dr. Angus’ research, funded principally by the NIH, focuses on clinical, epidemiologic and translational studies of sepsis, pneumonia, and multisystem organ failure and on health services research of the organization and delivery of critical care services. He has published several hundred papers, is section editor for “Caring for the Critically Ill” for JAMA, and the recipient of numerous awards.
Donald Yealy, MD
Chair of the Department of Emergency Medicine at the University of Pittsburgh School of Medicine and the University of Pittsburgh Medical Center

Dr. Don Yealy has focused most of his research on clinical decision making and the early care of many life-threatening conditions, including community-acquired pneumonia, sepsis, acute heart failure and respiratory failure. In 2009, he received the Outstanding Contribution in Research Award from the American College of Emergency Physicians for his significant contributions to the field. Keys to his work have been the following themes: How do we assess and treat acute illness? Can we do better? Locally, Dr. Yealy leads faculty in delivering care to nearly 1 million emergency department and urgent care patients each year. He is also a leader in hospital and health system quality efforts and the author of over 300 scientific publications.
Clifton Callaway, MD, PhD
Professor of Emergency Medicine; Executive Vice-Chairman of Emergency Medicine; Ronald D Stewart Endowed Chair of Emergency Medicine Research

Dr. Clif Callaway studies resuscitation medicine with special emphasis on brain injury after cardiac arrest. He has developed a translational research program devoted to the topic of resuscitation from sudden death. Emphasizing the continuity of care during resuscitation, he has collaborated with prehospital care providers and emergency physicians to study acute cardiac interventions, developed a platform to study intensive care interventions, and worked with partners in rehabilitation to study long-term outcomes after cardiac arrest. Work in prehospital care has led to studies about acute monitoring and regionalization of care.
Christian Martin-Gill, MD, MPH
Assistant Professor of Emergency Medicine

Dr. Martin-Gill is an Assistant Professor in the Department of Emergency Medicine at the University of Pittsburgh School of Medicine. He is Associate Medical Director of STAT Medevac and UPMC Prehospital Care, as well as Associate Program Director of the UPMC Emergency Medical Services (EMS) Fellowship. He works clinically as an attending physician at the UPMC Mercy Emergency Department. Dr. Martin-Gill's academic focus is in the evaluation and management of acute care conditions in the prehospital setting, optimizing regionalized systems of care for acute care conditions (e.g. STEMI, cardiac arrest, sepsis), and the development of national evidence-based guidelines for EMS. Dr. Martin-Gill received his medical degree from the University of Virginia and completed an Emergency Medicine residency and EMS fellowship at the University of Pittsburgh Medical Center.
Educational Resources
Sepsis Fact Sheet from the National Institute of General Medical Sciences
Sepsis Information from the Centers for Disease Control and Prevention
ThinkSepsis in the Press
Spot Sepsis: How New Tool Could Speed Help (EMS World, John Erich, 4/9/14)
University of Pittsburgh
University of Pittsburgh Department of Emergency Medicine
University of Pittsburgh Department of Critical Care Medicine
Pitt Innovation Challenge (PInCh)
Organizations for Sepsis Awareness
Stories
Rory Staunton: A young boy from Queens, New York whose death from sepsis created a nationwide movement to address the issue of childhood sepsis and its treatment.
Erin Flatley: A 23-year-old girl who died of sepsis six days after going to the hospital for a simple surgical procedure. Her father, Carl Flatley, became a driving force in the fight against sepsis and founded the Sepsis Alliance in 2004.
The Faces of Sepsis: Tributes, stories of survival, and stories from healthcare professionals who share why sepsis awareness is important to them.
References
Merinoff Symposium 2010: Sepsis; Feinstein Institute for Medical Research
Gaieski DF, Edwards JM, Kallan MJ, et al. Benchmarking the incidence and mortality of severe sepsis in the United States. Crit Care Med 2013; 41:1167-1174
Seymour CW, Rea TD, Kahn JM, et al. Severe Sepsis in Prehospital Emergency Care: Analysis of Incidence, Care, and Outcome. Am J Resp Crit Care Med, 2012
Seymour CW, Carlbom D, Engelberg RA, et al. Understanding of Sepsis among Emergency Medical Services: A Survey Study. J Emerg Med, 2011
Suffoletto B, Frisch A, Prabhu A, et al. Prediction of serious infection during prehospital emergency care. Prehosp Emerg Care 2011; 15:325-330
Seymour CW, Kahn JM, Cooke CR, et al. Prediction of critical illness during out-of-hospital emergency care. JAMA 2010; 304:747-754
Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med 2003; 29:530-538
$20
Level 1
Your gift will help move the ThinkSepsis project forward. Thank you for supporting our mission!
$30
Level 2
With this gift, we can purchase a protective case and cover for one secure alert device.
$70
Level 3
This gift will support two months of a wireless contract for an EMS truck participating in the pilot test.
$105
Level 4
Giving at this level will provide a full 3-month wireless contract for one secure device.
$265
Level 5
With this gift, we can get halfway to providing an EMS truck with a secure alert device for the pilot test (16GB iPad Wi‑Fi + Cellular).
$530
Level 6
This generous gift will provide one secure alert device for the pilot test (16GB iPad Wi‑Fi + Cellular).
$665
Level 7
Your incredible gift will support fully equipping one EMS truck with the complete sepsis alert system for the pilot test, including a secure device, case, cover and wireless contract.